Gateways: International Journal of Community Research and Engagement
Vol. 17, No. 1
August 2024
PRACTICE-BASED ARTICLE
Building Research and Evaluation Within an Australian Community Eating Disorder Organisation Through Academic Partnership: A Pragmatic Protocol
Sumedha Verma PhD1,2, Caroline Salom PhD3, Jane Miskovic-Wheatley DPsych(Clin)1, Phillip Aouad PhD1, Morgan Sidari PhD1,4, Belinda Caldwell MPH2 and Sarah Maguire PhD1
1 InsideOut Institute for Eating Disorders, Central Clinical School, Faculty of Medicine & Health, The University of Sydney, New South Wales, Australia
2 Eating Disorders Victoria, Victoria, Australia
3 Institute for Social Science Research, The University of Queensland
4 Queensland Eating Disorder Service, Metro North Hospital and Health Service, Queensland Health, Queensland, Australia
Corresponding author: Dr Sumedha Verma, sumedha.verma@eatingdisorders.org.au
DOI: https://doi.org/10.5130/ijcre.v17i1.9145
Article History: Received 16/05/2024; Revised 11/07/2023; Accepted 16/07/2024; Published 08/2024
Abstract
Eating disorders are complex mental health conditions with rising prevalence. Despite this, research and evaluation (R&E) remain under-funded, hindering translation, policy, prevention and advances in care; an equitable and responsive ecosystem of research and knowledge-sharing across the sector is needed to enhance outcomes for people and systems affected by eating disorders. Community members engage with community eating disorder organisations/services to receive guidance and support, often through innovative co-designed programs and resources. Building R&E capacity and capability within community settings is essential in capturing, leveraging and translating local knowledges, such as evaluation outcomes to research, policy, practice settings and the broader community to improve understandings, actions and outcomes. Partnerships between community service providers and academic researchers could be a way of establishing reciprocal knowledge-sharing pathways while simultaneously building internal R&E capacity/capability. The current article presents a longitudinal participatory protocol to plan for, co-design and implement R&E practices within an Australian community-based eating disorder service via an academic partnership. We present a four-stage methodological outline aiming to (a) identify the needs, experiences and feasibility of engaging in R&E in a community eating disorder context; and (b) collaboratively plan for, develop and integrate R&E practices through partnership. We will collect data through focus groups, meetings, interviews, researcher notes and questionnaires across several months. This pragmatic plan can guide future collaborative R&E building efforts within a community mental health context in ways that inform the development and scalability of sustainable, effective and efficient R&E praxis and partnerships across the eating disorder and broader mental health sector.
Keywords
Eating Disorders; Research and Evaluation; Capacity and Capability Building; Community-Academic Partnership; Community-Based Participatory Research; Co-Design
Introduction
Eating disorders are complex conditions that have a rising prevalence and systemic impacts (Ágh et al. 2016; Butterfly Foundation 2024; Hay et al. 2023; Johns et al. 2019). Despite this, funding for eating disorders research remains notoriously limited compared to other mental health conditions (All-Party Parliamentary Group 2021; Bryant et al. 2023). Pervasive and persistent gaps in research and evaluation (R&E) systems within and across the eating disorder sector hinder the creation, collection and translation of important knowledges. Strengthening an equitable and responsive ecosystem of knowledge-sharing to enable the multi-directional flow of information between community, research, policy and practice settings would (a) capture and uplift diverse community voices and experiences; (b) narrow the notable research–practice gap (Robinson et al. 2020); and (c) inform policy, prevention and treatment frameworks, and ultimately improve outcomes for communities and systems impacted by eating disorders.
Community members engage with eating disorder organisations/services in the community that provide information, advocacy, guidance and support, serving as the gateway to local knowledges such as consumer demographic data and feedback. Rich information (data) that may be created and captured at the community level could be (a) linked with state-level, national and international data to build an evidence base; (b) inform the development and delivery of future innovations; (c) support funding applications; and importantly (d) identify and address areas of community need, such as marginalised/under-serviced communities (Clark et al. 2023; National Eating Disorders Collaboration 2023). This holds implications for individual consumers, families and communities, and the broader healthcare system (Kaufman et al. 2020).
In community eating disorder settings, lived experience and peer work is increasingly becoming a central facet of organisational delivery, in that programs/services are co-designed and delivered by lived experience peers (Eating Disorders Victoria 2023; Utpala et al. 2023). This spurs innovation, such as early intervention and peer-based supports outside of clinical and research settings. R&E practices are integral to demonstrate the effectiveness, efficiency, value and merit of such programs/services, and in translating them across settings to support others. Yet in the context of under-resourcing, requisite R&E cultures, capacity and capability within eating disorder community services remain limited, as do connections with research settings in leveraging these important data.
Uplifting R&E in community services has been recommended by two ten-year national eating disorder strategies (InsideOut Institute 2021; National Eating Disorders Collaboration 2023). Establishing pathways between community services and research settings through academic partnership could be a promising way of enabling knowledge-sharing and learning and building organisational R&E capability (Farmer & Weston 2002; Golenko et al. 2012). Community-Based Research is a form of Participatory Action Research (Minkler & Wallerstein 2008) which involves partnerships between researchers and community stakeholders to collaboratively identify and find ways of addressing issues faced by the community itself (Wallerstein and Duran 2006). By attempting to de-centre research ownership through democratic processes, community partners take an active role in decision-making and engaging in research practice alongside research partners, with both sides sharing their unique skills, knowledge and expertise to learn and mutually benefit from one another to bring about social change (Israel et al. 2018; Jull et al. 2017; Wilson 2019). Community-academic partnerships have been described previously (e.g., April et al. 2023; Morton et al. 2014), and guidelines on sharing power, enhancing equity and enabling systemic change are available (Sadler et al. 2012).
Engaging in community-based R&E seems particularly relevant for largely consumer-based or lived-experience-led organisations because service providers often belong to the community they serve. This can facilitate decision-making and promote advocacy efforts (Reed 2015), lead to better understandings and recommendations (Guijt 2014), and ultimately promote community ownership of research/evaluative processes and outcomes (April et al. 2023; Israel et al. 2012). Additionally, as financial resources to support external evaluation can often be limited within community services, strengthening the capability and capacity of service providers to systematically collect and monitor consumer information, and to evaluate, learn from and shape their own service delivery may represent a more sustainable and cost-effective way of engaging in R&E.
Here, as research and community partners, we specifically aim to place community-engaged R&E in an eating disorder context. To do so, we present a pragmatic methodological plan to collaboratively build and integrate R&E practices through a community-academic partnership into a real-world community eating disorder organisation with limited existing infrastructure. At the same time, we will provide a plan to identify the needs, enablers, challenges and opportunities of engaging in R&E to inform sustainable practices into the future. In documenting the plan, processes, experiences and learnings of the partnership and R&E building, we offer a guide to service providers, researchers, policymakers and other relevant stakeholders. This aims to enhance R&E cultures, capability and capacity at the community level to facilitate greater knowledge sharing, empowerment and innovation within, across, and beyond the eating disorder sector.
Context
Overview of Eating Disorders
Eating disorders are encompassing in that they impact a person’s emotional, mental, physical and social wellbeing (Berkman et al. 2007; Miskovic-Wheatley et al. 2023). They are systemic in that they impact upon others, such as caregivers and families Fletcher et al. 2021; Karlstad et al. 2022). While evidence-based treatments exist, cost, stigma and shame, lack of access to and accessibility of care and limited knowledge may delay people seeking and receiving timely help (Hamilton et al. 2022; Regan et al. 2017), reflecting key issues in the current healthcare climate for people affected by eating disorders and those who support them.
Current Project
This project is part of a larger, multi-year research project to leverage multidisciplinary eating disorder research across Australia (‘Mainstream’; www.mainstreamresearch.org.au/), which was funded by the National Health and Medical Research Council’s Medical Research Future Fund Million Minds Mission Grant (APP1178922). This project also funded a full-time post-doctoral researcher, to be based ‘on the ground’ at EDV, as a primary research partner, who is also part of a larger academic team at the InsideOut Institute for Eating Disorders, which is affiliated with the University of Sydney and Sydney Local Health District. Other researcher partners include the academic co-authors of the current article, and other researchers affiliated with the InsideOut Institute who may provide research-related support and guidance. Recruitment of community partners began in August 2023; the project end date is expected to be
mid-2024.
Community Service Setting
Community eating disorder organisations provide opportunities for community members to engage in support prior to, in tandem with, and/or beyond tertiary healthcare settings, given that treatment of an eating disorder can be arduous and challenging (Conti et al. 2021; McArdle 2019; Solhaug Storli & Alsaker 2021). Eating Disorders Victoria (EDV) is an Australian community-based not-for-profit organisation that provides advocacy and support for people experiencing or caring for someone with an eating disorder. Support is available broadly through telehealth counselling and nursing, various support groups and programs, comprehensive e-learning courses, resources and linkage to external services.
Peer-based supports, normally developed within community services like EDV, represent innovative pathways to enhance people’s wellbeing and recovery (Lewis & Foye 2021) and have been strongly recommended within general mental health settings and specifically within the eating disorders context (Commonwealth of Australia 2013; National Eating Disorders Collaboration 2023; State of Victoria 2023). In this way, community services present novel and unique opportunities to facilitate connections between community members and lived experience peers, alongside and beyond traditional eating disorder treatment, in efforts to validate people’s experiences and further support their mental health, wellbeing and recovery (National Eating Disorders Collaboration 2019; State of Victoria 2023).
The Carer Coaching Program
The Carer Coaching Program is an eight-week, peer-led early intervention support program offered at EDV for caregivers of a young person diagnosed with a restrictive eating disorder (i.e. anorexia nervosa, atypical anorexia, avoidant restrictive food intake disorder) and currently on a waitlist to commence formal treatment. The program was co-designed in early 2020 by a group of lived experience carer consultants and EDV service providers in response to long waitlists to access treatment services during the COVID-19 pandemic. People with lived experience of caring for a young person with an eating disorder were responsible for developing most of the program content. Two of them had expertise in program design and clinical governance. Program content then underwent a review process with senior managers within the organisation prior to delivery. The program is facilitated by lived experience peer workers (‘Carer Coaches’).
Key components of the Carer Coaching Program include peer-based support, psychoeducation around eating disorders and evidence-based treatments, basic meal support (not dietary advice), emotional regulation strategies, self-care and managing fatigue, and provision of appropriate resources. These components draw on prior interventions by carers of young people with an eating disorder, including peer-led (e.g., Grennan et al. 2022), clinician-led (e.g., Gisladottir et al. 2017; Kurnik Mesarič et al. 2024) and self-directed (Truttmann et al. 2020) interventions.
While Carer Coaches undertake regular professional development training, it is made clear to program participants that they offer peer-based guidance and support, not clinical perspectives. Content is flexibly delivered in a personalised manner to address unique support needs of program participants. While session-by-session outlines exist, these serve as general practices; in practice, the order of session delivery may change in order to deliver more pertinent information sooner. This type of flexible, tailored delivery is common across EDV’s programs and services promoting personalised care. All sessions are delivered remotely via Zoom software. Following sessions, Carer Coaches send follow-up emails to program participants with a summary of the key points and materials used in the sessions, as well as any relevant additional resources (e.g. handouts, websites).
Carer Coaches engage in monthly supervision with a manager, who is also a mental health clinician, in addition to ad hoc consultation when additional needs emerge. They also attend weekly multidisciplinary team meetings and regular lived experience group supervision. Collectively, supervision and consultations provide opportunities to discuss the suitability of participation, risk and ethical practice management, plan sessions and discuss challenging cases, engage in reflective practice and to receive emotional support.
Methods
Community-Academic Partnership
A community-academic partnership will be established and maintained across multiple and varied points of engagement over approximately 12 months to jointly co-plan, co-design, implement, monitor and evaluate R&E practices of the Carer Coaching Program. As the primary research partner, co-author Verma will contribute her professional expertise by sharing her knowledge of ethical, practical and methodological considerations around R&E. Those employed within a directorial, managerial or service provision role within EDV and have close involvement with the Carer Coaching Program will be invited to take part, read an explanatory statement and provide informed consent (see Appendices 1 and 2). As community partners, service providers will be invited to contribute their expertise and unique local knowledge of community needs, and personal, organisational and contextual factors, which may include prior R&E knowledge. Community partners will also be encouraged to take an active role in developing and undertaking research evaluation practices. This may include sharing ideas, engaging in decision-making during meetings with the primary research partner and engaging in the development and review of emerging R&E processes and materials. Appendix 3 lists anticipated roles and responsibilities of partners.
Design
This project adopts a longitudinal community-based participatory framework. To assist with engaging in interactive and iterative co-design processes with community partners, we will be guided by existing community-engaged R&E methodologies and guidelines (e.g., April et al. 2023; Banks et al. 2013; Israel et al. 2012; Jull et al. 2017; Kaufman et al. 2020; Reed 2015; Sadler et al. 2012). Additionally, we use frameworks from the Centers for Disease Control and Prevention (CDC, 1999) and the New South Wales Treasury (NSW, 2013), which collectively outline the steps, standards and principles of effective evaluation practice. Community partners are not reimbursed as engagement occurs during their normal working hours.
Data Collection
Data is collected via mixed methods, including meetings, semi-structured interviews, questionnaires, researcher notes and tracking sheets. Researcher notes include information such as points of engagement with community partners, methodological discussion points and outcomes, a reflexive log of personal reflections and insights, and any potentially impactful events (Lincoln & Guba 1985). Reflexive journaling is designed to facilitate greater researcher insights and understandings (Janesick 1999), and will give research partner(s) the ability to document needs, barriers and enablers throughout the project. Community partners will also complete questionnaires, which are discussed in detail below.
Positionality
As co-authors, our ontological (i.e. social constructionist, participatory) and related epistemological orientations will inevitably impact project design and arising interpretations because constructionism is an interpretivist ontological paradigm in which realities are intersubjective and relative, and are co-constructed through dynamic social processes (Berger & Luckmann 1967; Merriam & Brockett 2007). As Overton (2017; p. 1209) puts it, through a social constructionist lens, ‘we come to know what is real through our shared interaction with the environment and the others who share that environment with us, at different moments in our time’. All co-authors have previously engaged in co-design within community-based settings: six of us hold doctoral-level qualifications, five of us identify as holding lived experience of an eating disorder or caring for someone with one, three of us identify as coming from non-White backgrounds, three of us are early-career researchers, four of us are psychologists, and two of us identify as being queer.
Community-based participatory research seems imbued with constructivist beliefs in which knowledge and meaning are co-created through collaborative and social processes (Peralta & Murphy 2016), highlighting the role of power in study design and decision-making (Corrigan & Oppenheim 2023). To encourage awareness of how unique backgrounds, biases and assumptions may impact project processes and outcomes, we prioritise reflexive practices, such as engaging in reflexive journaling and supervision (Banks et al. 2013).
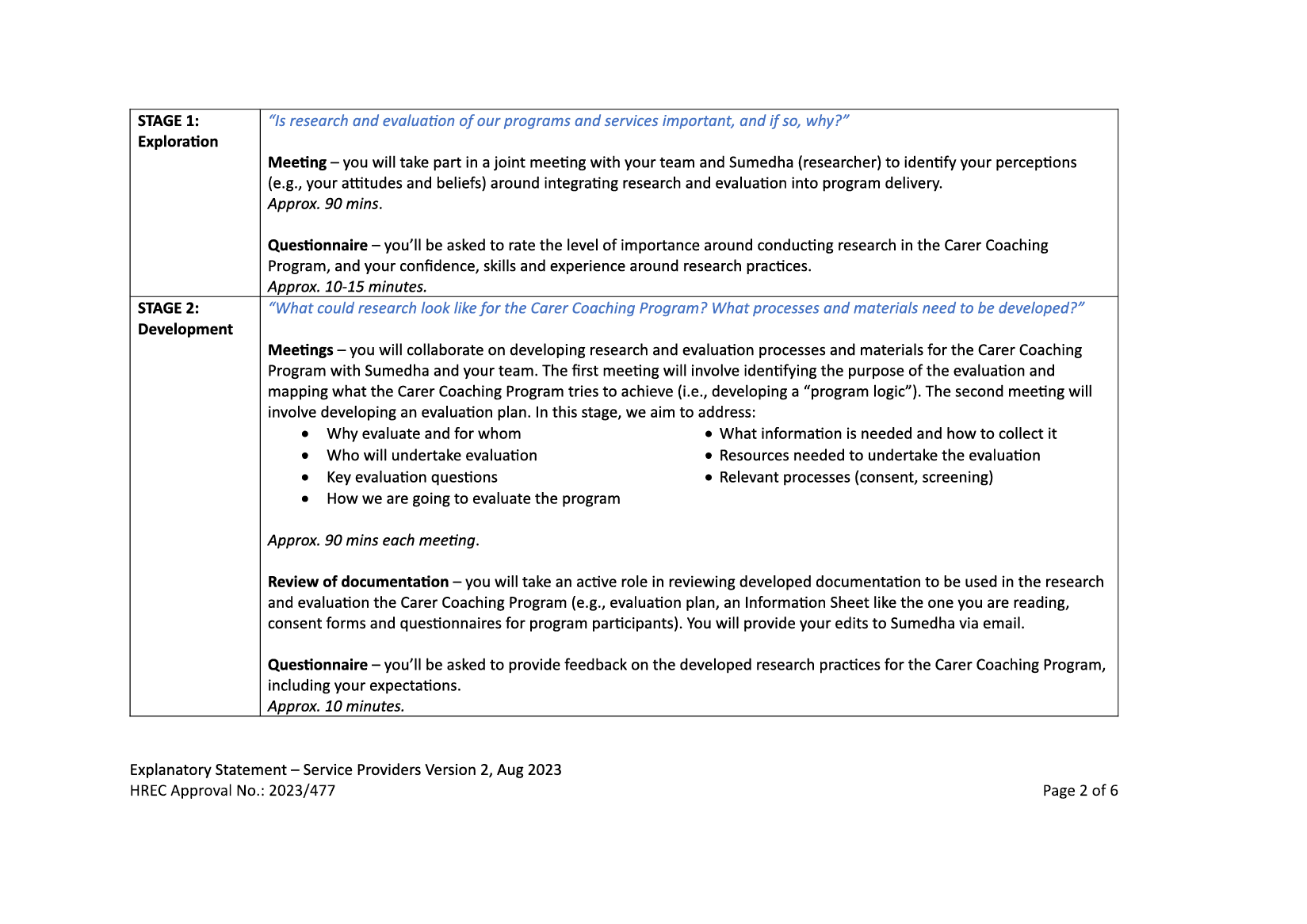
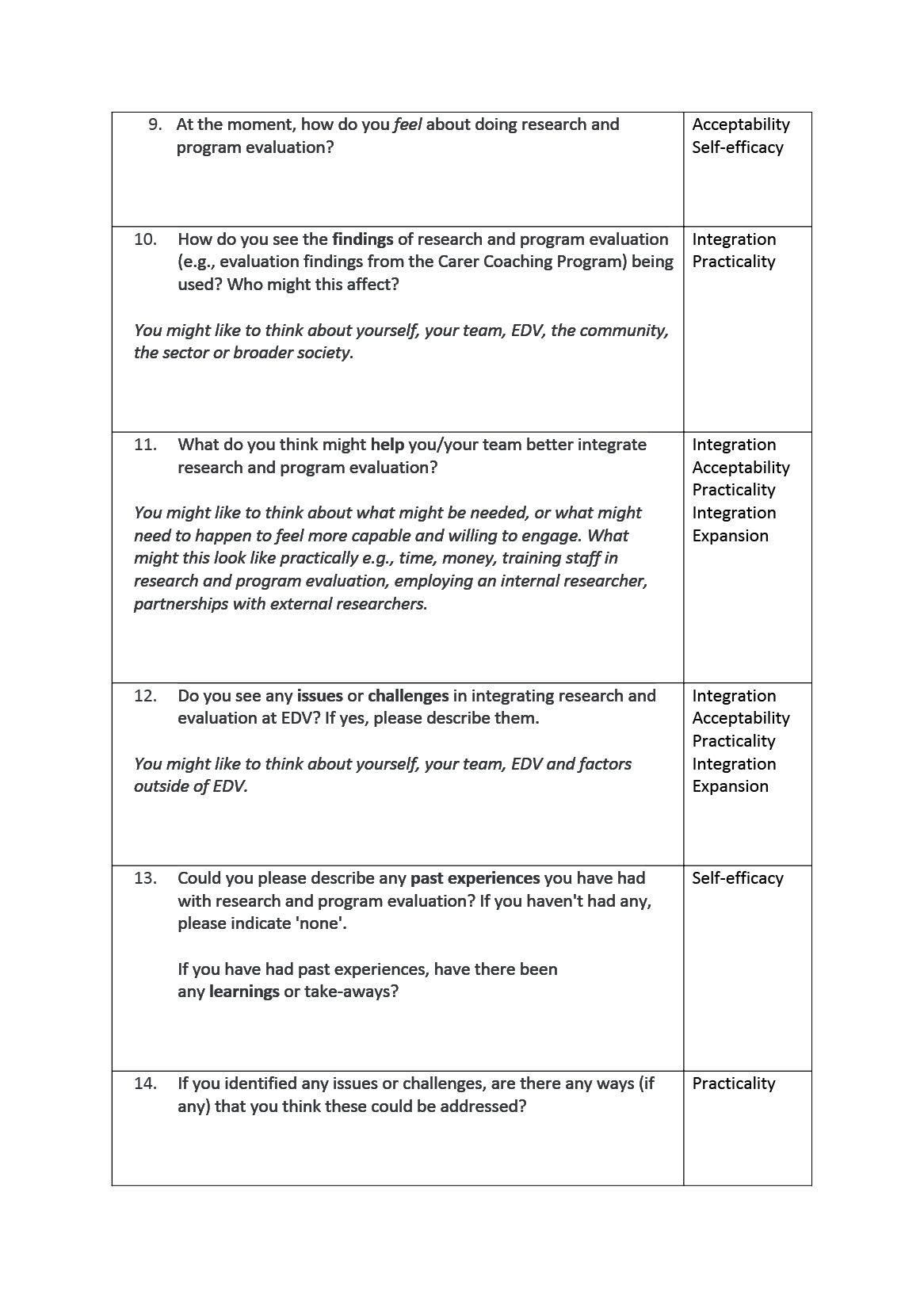
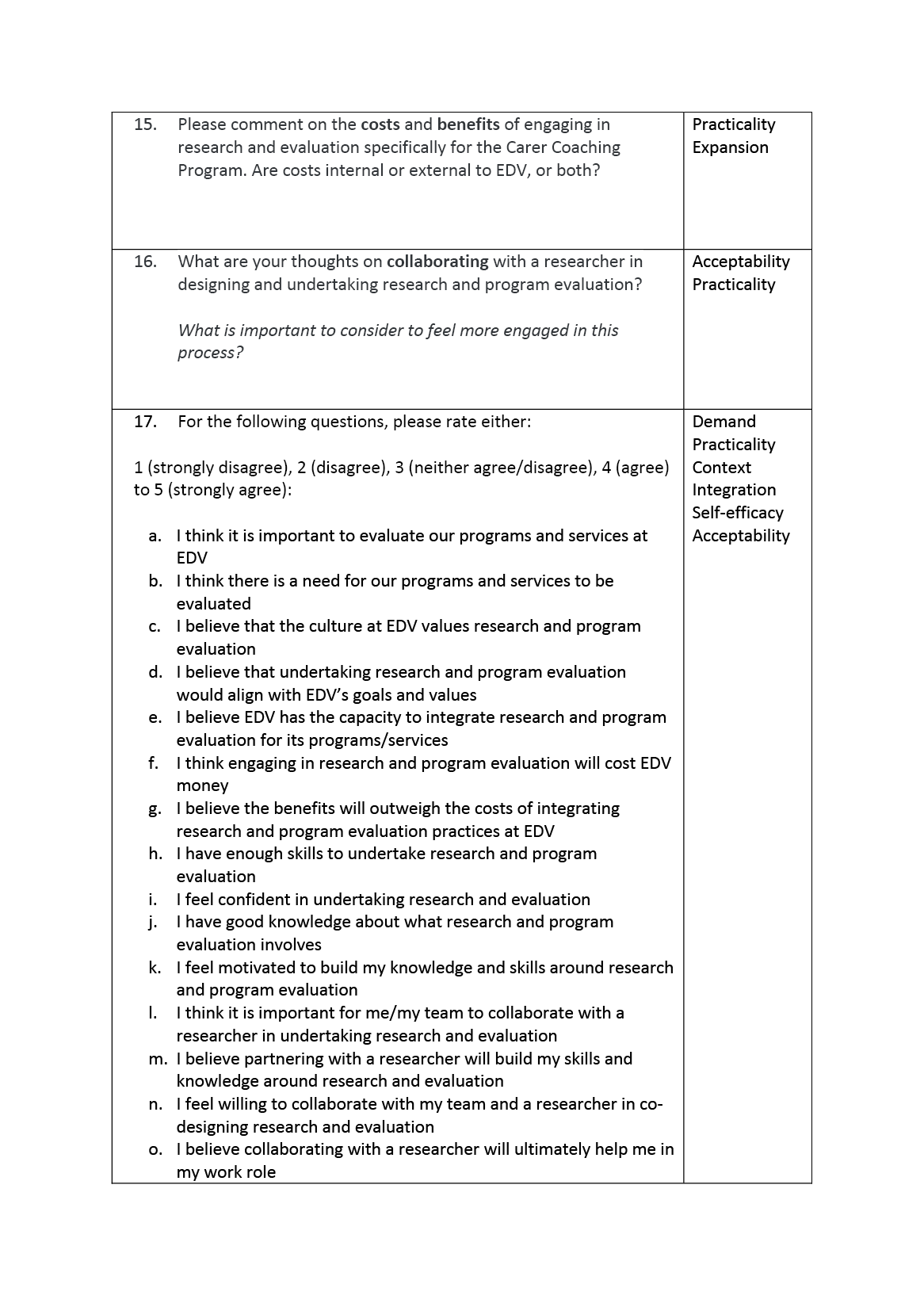
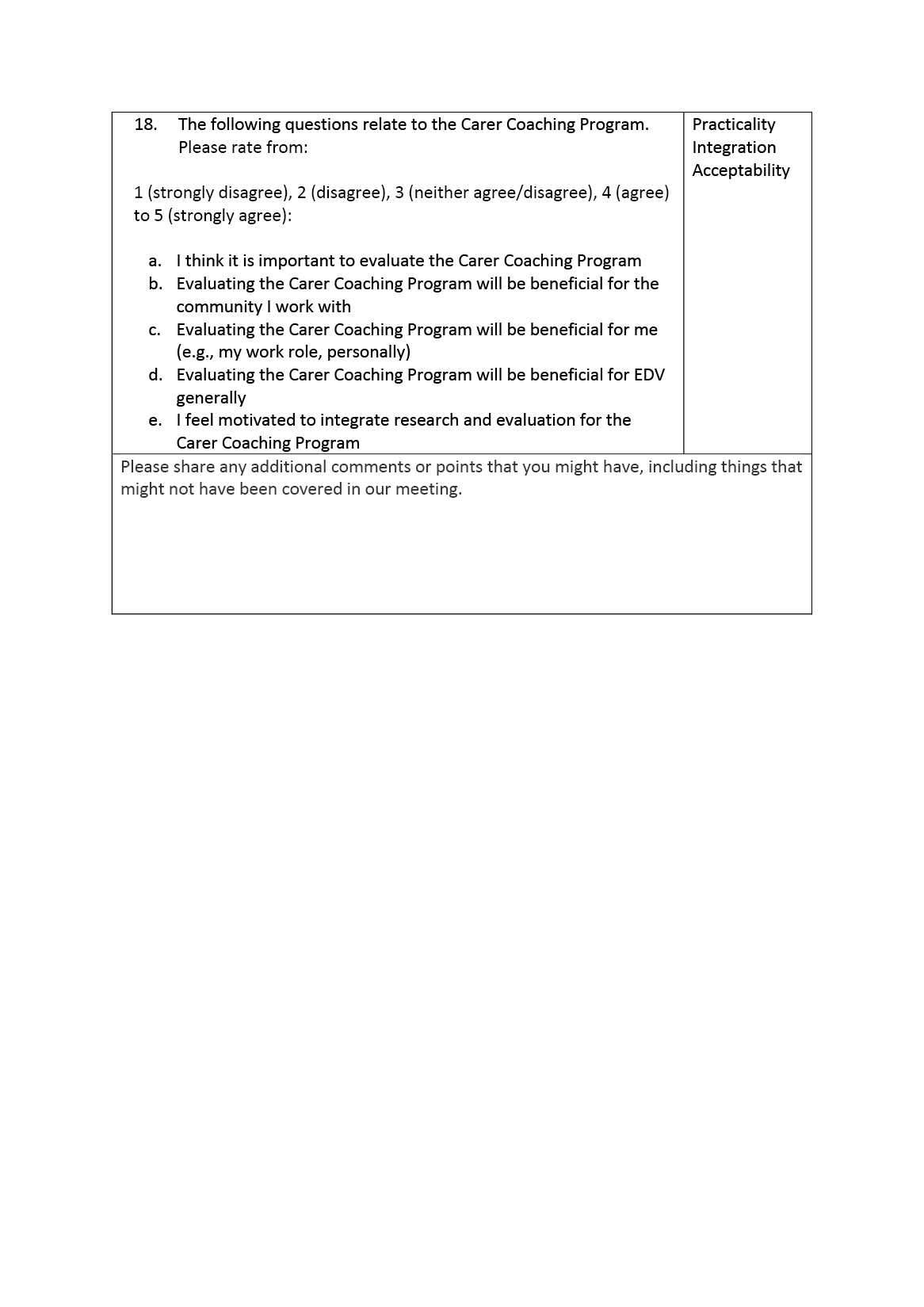
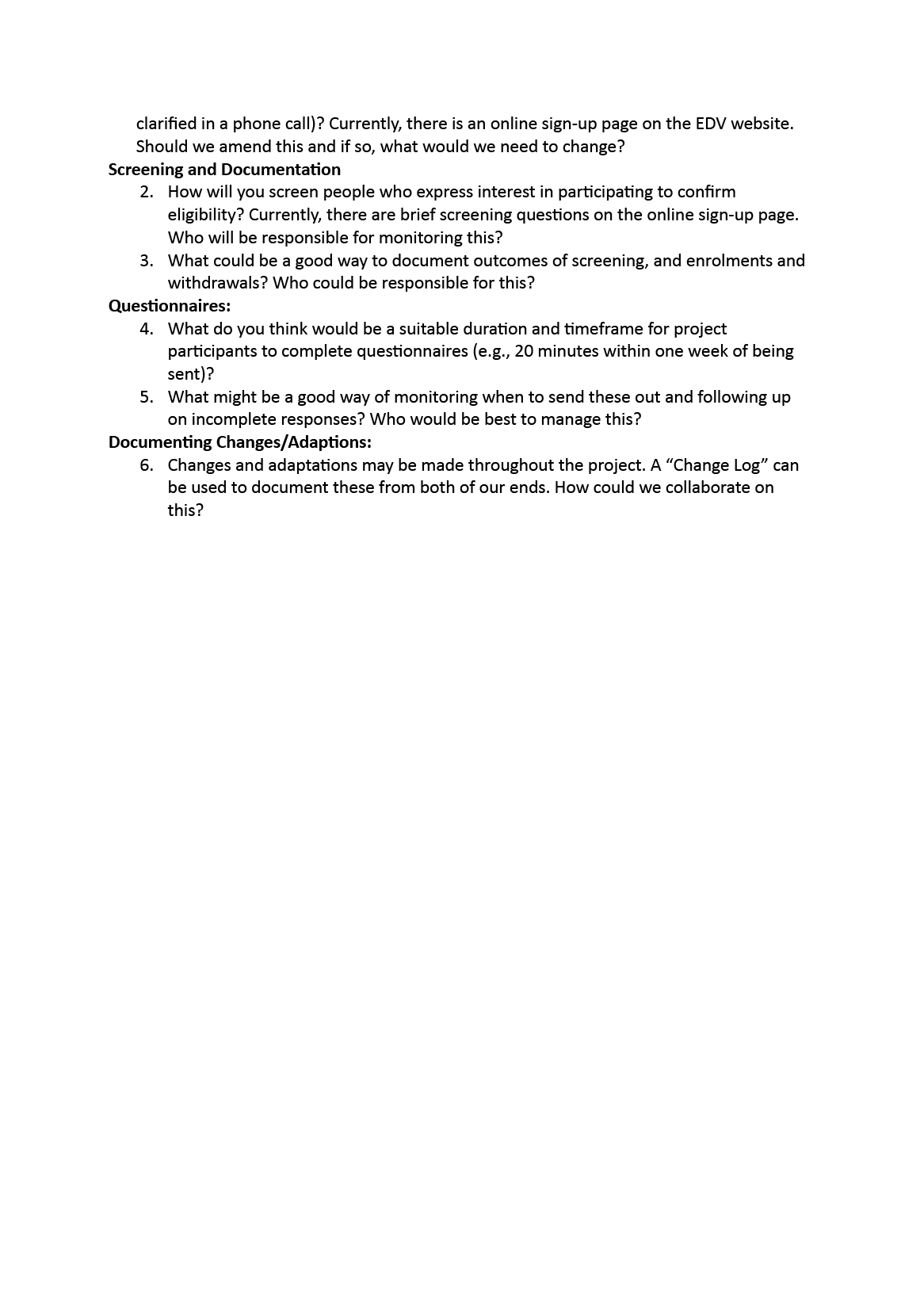
Procedure
Our project will unfold over four stages (see Figure 1). Each stage includes its own meeting guide and questionnaire to assess individual, interpersonal, community, organisational and systemic factors impacting R&E (see Appendices). Community partners will be invited to attend all meetings throughout the project period, which will be facilitated by the primary research partner. The duration of each meeting will be 90 minutes unless otherwise noted and may be undertaken either in person at the EDV office or via videoconferencing.
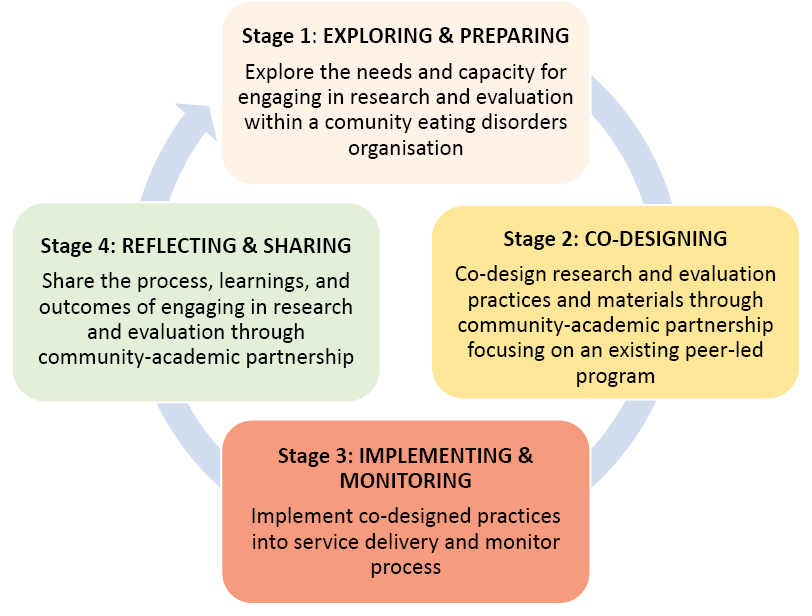
Figure 1. Project Stages to Build and Integrate Research and Evaluation within a Community-based Eating Disorder Setting through Academic Partnership
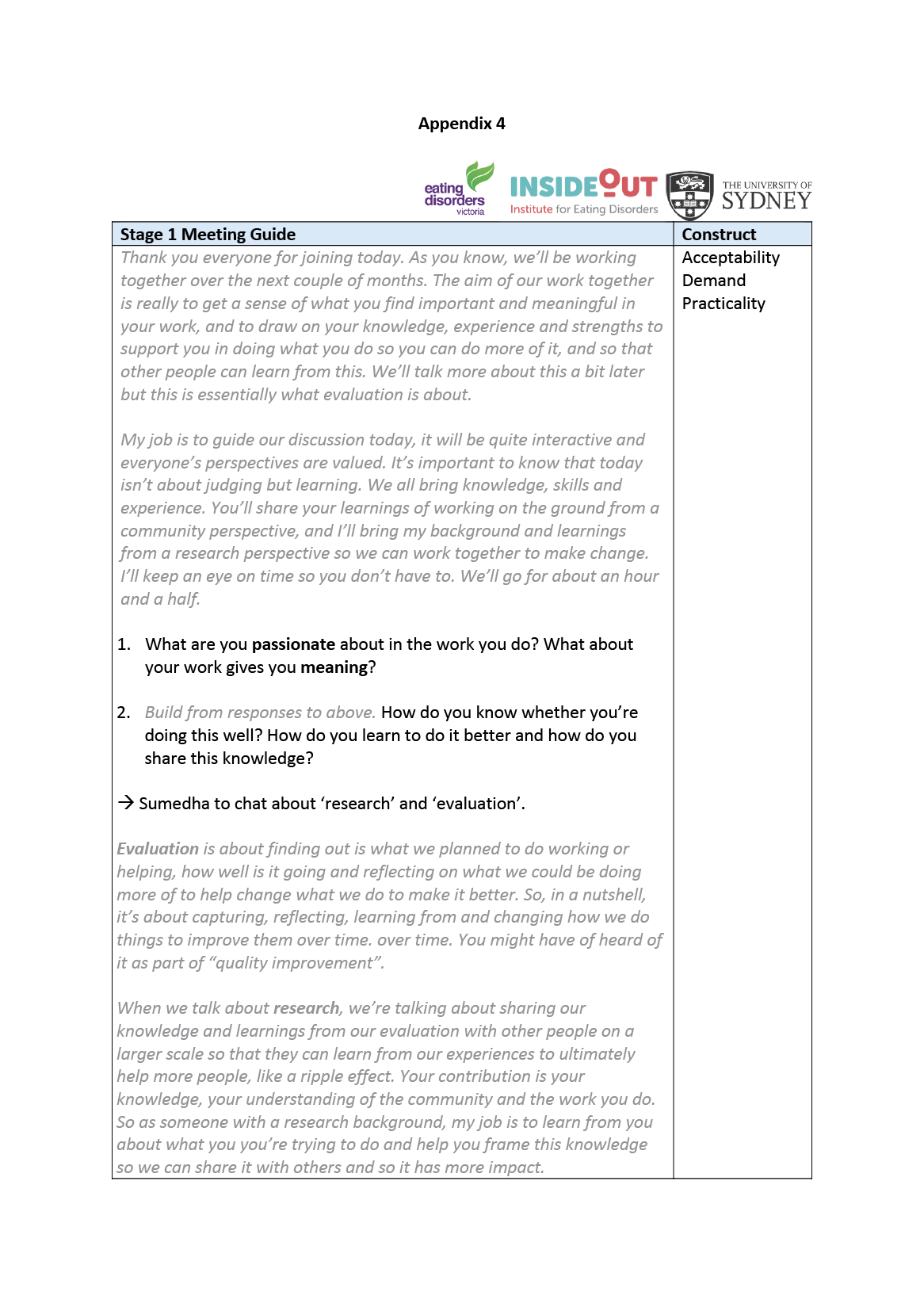
Stage 1: Exploration of Research and Evaluation Needs and Capacity, and Preparing for Co-Design
During Stage 1, community and research partners will engage in an initial meeting to identify the needs, capacity, capabilities, motivation, expected outcomes and other enablers/challenges of undertaking and implementing R&E within service delivery (see Appendix 4). Community partners will complete a questionnaire involving quantitative ratings and qualitative questions around R&E capacity, capability and building for example, ‘Do you see any benefits or advantages of doing research and program evaluation?’ and ‘What are your thoughts on collaborating with a researcher in designing and undertaking research and program evaluation?’ (see Appendix 5).
Stage 2: Collaborative Development of Research and Evaluation Practices and Materials
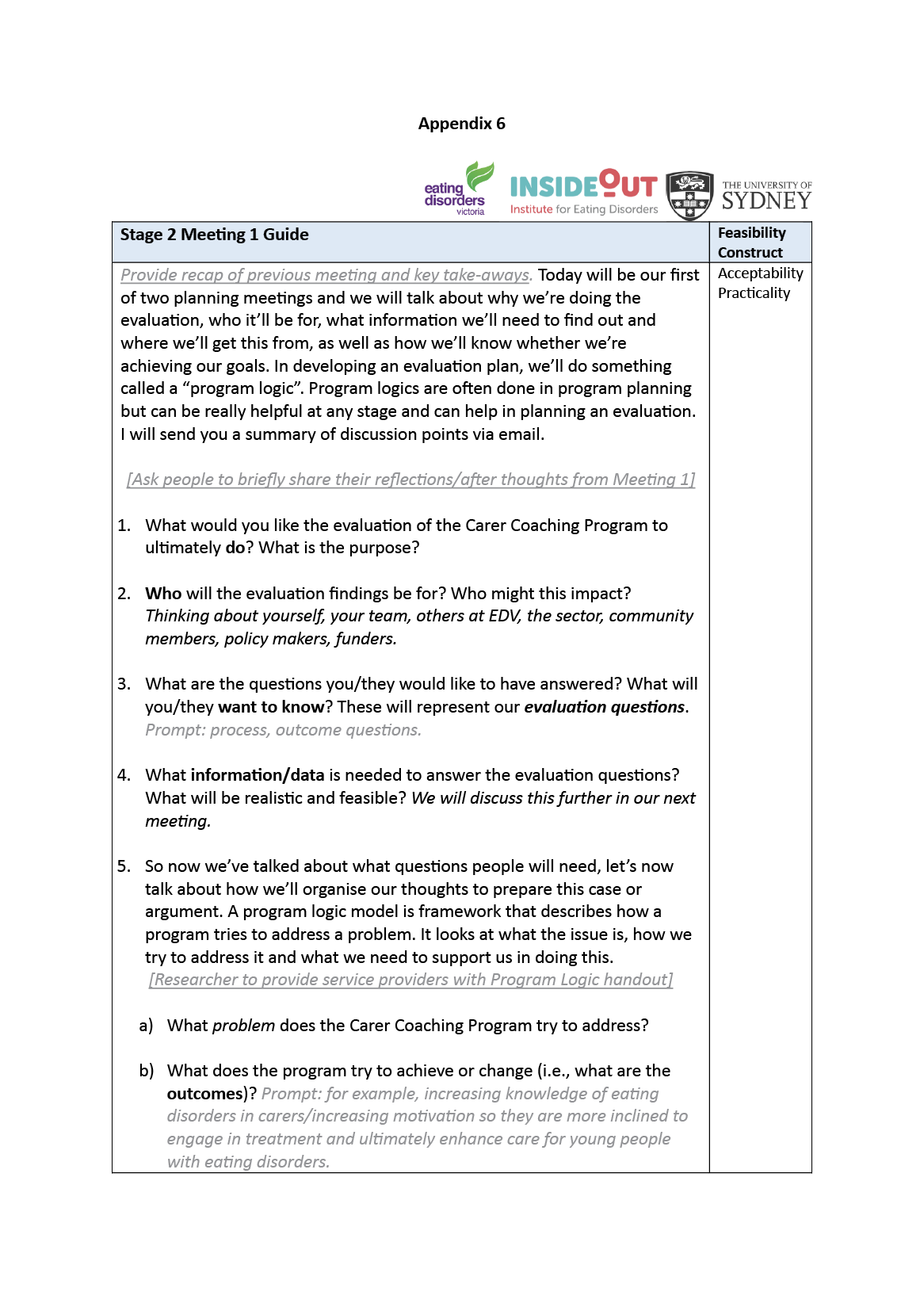
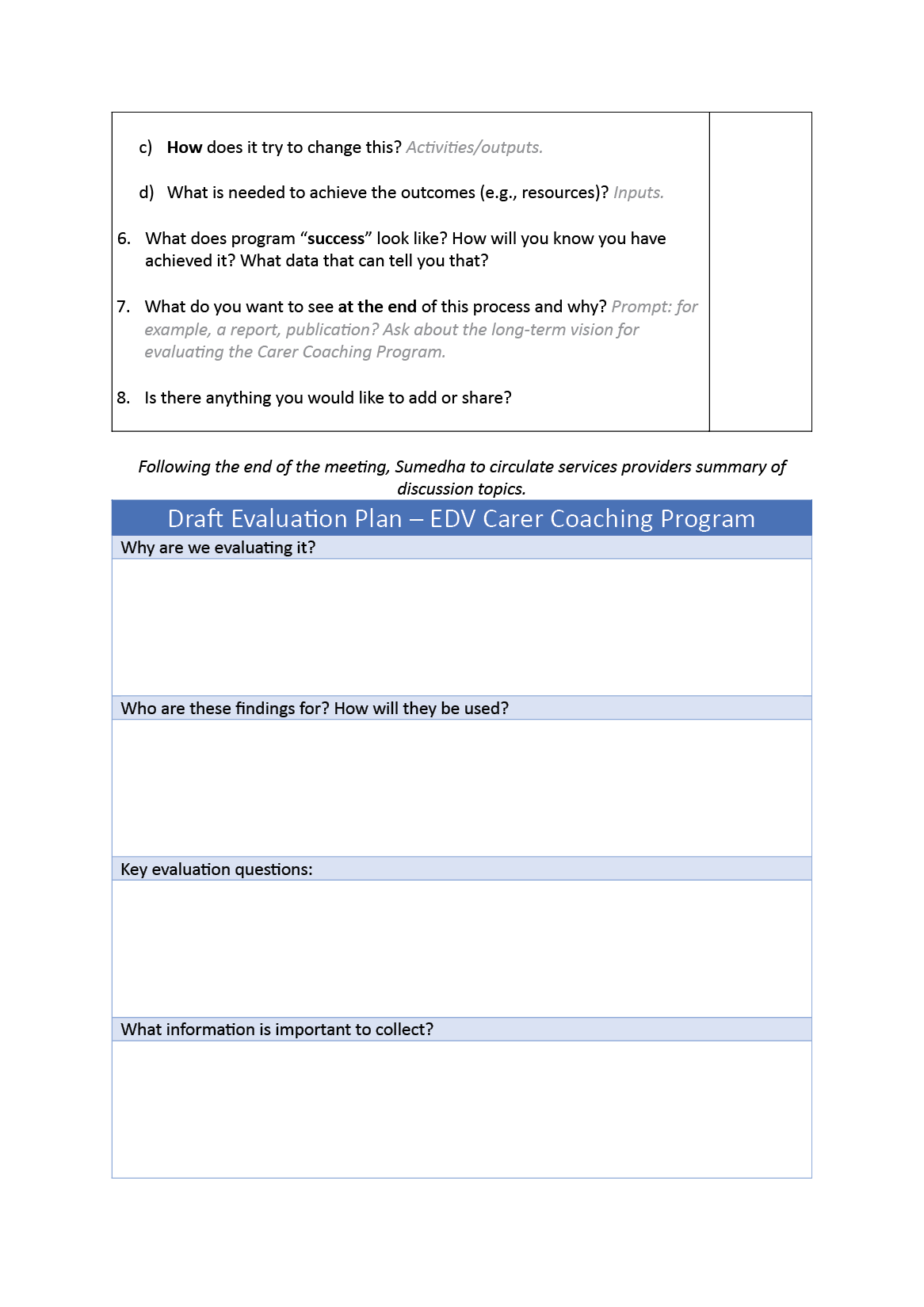
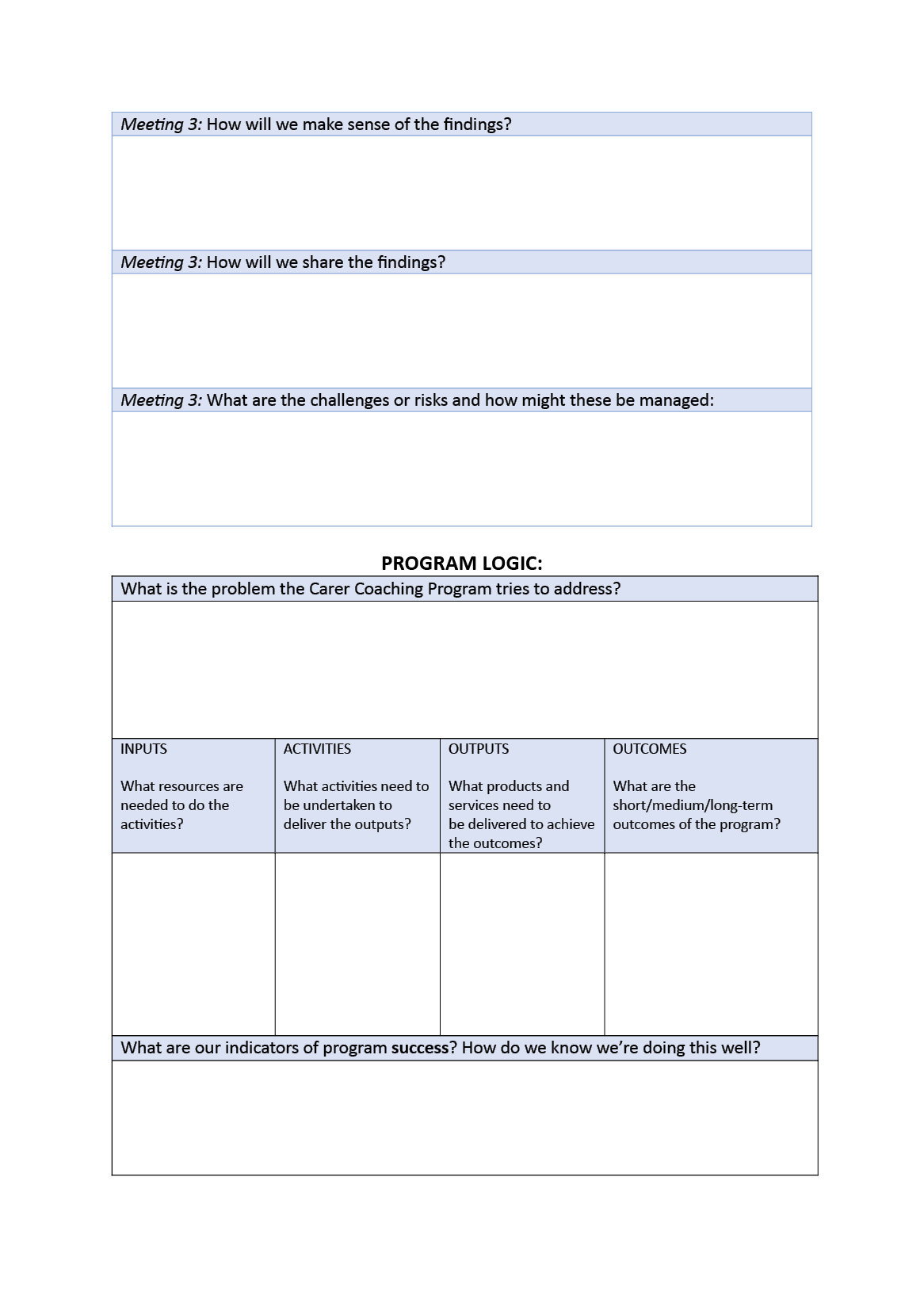
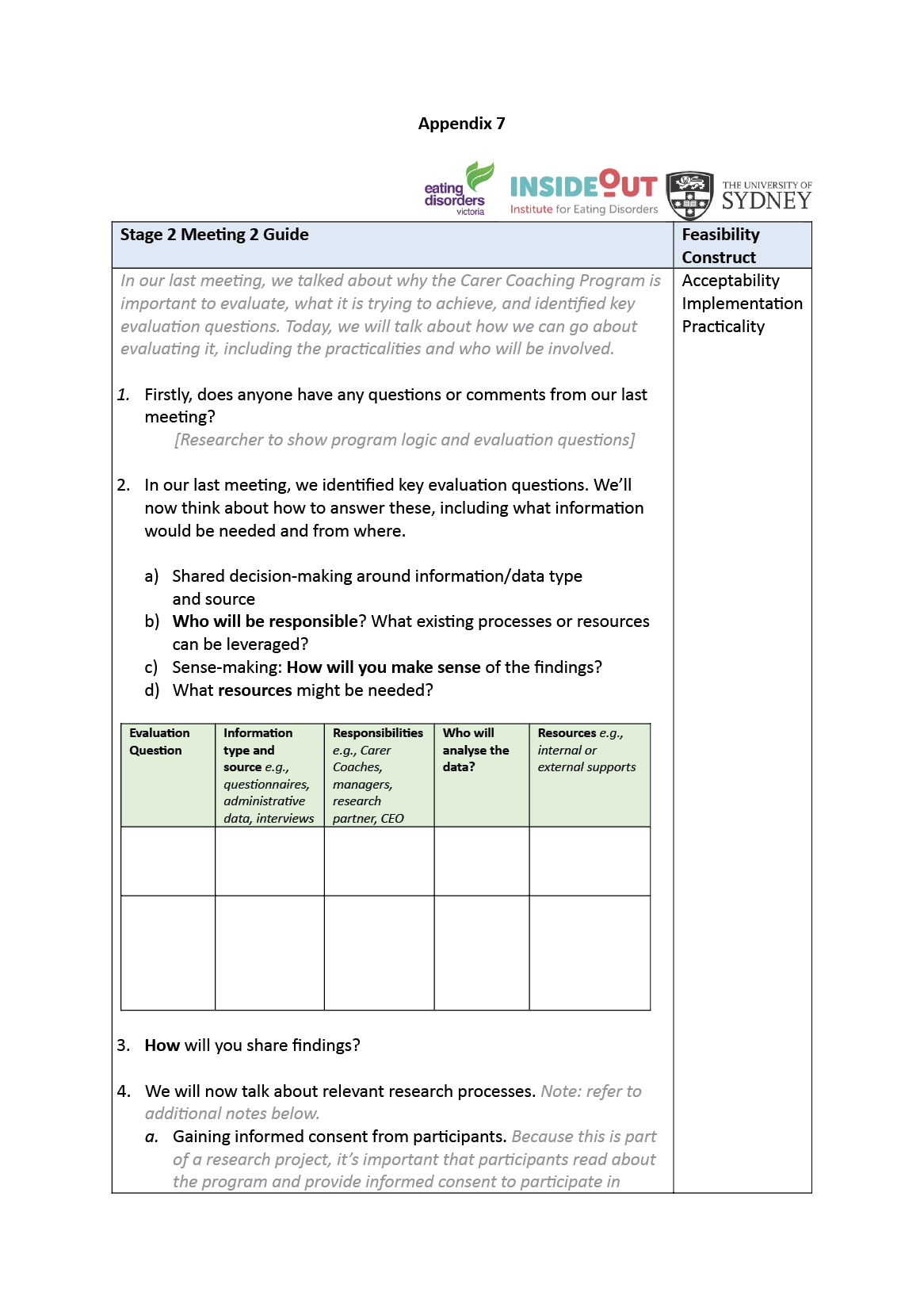
Building on responses gained during Stage 1, R&E practices and materials for the Carer Coaching Program will be co-designed in Stage 2 via shared decision-making through meetings and iterative reviews by community and research partners (see Appendices 6 and 7). The purpose of this stage is two-fold (a) to build knowledge and skills around R&E among community partners through knowledge-sharing (e.g. ethical considerations such as informed consent, steps involved in program evaluation, gathering/analysing data via mixed methods); and (b) to collaboratively develop R&E practices and materials to be integrated into service delivery.
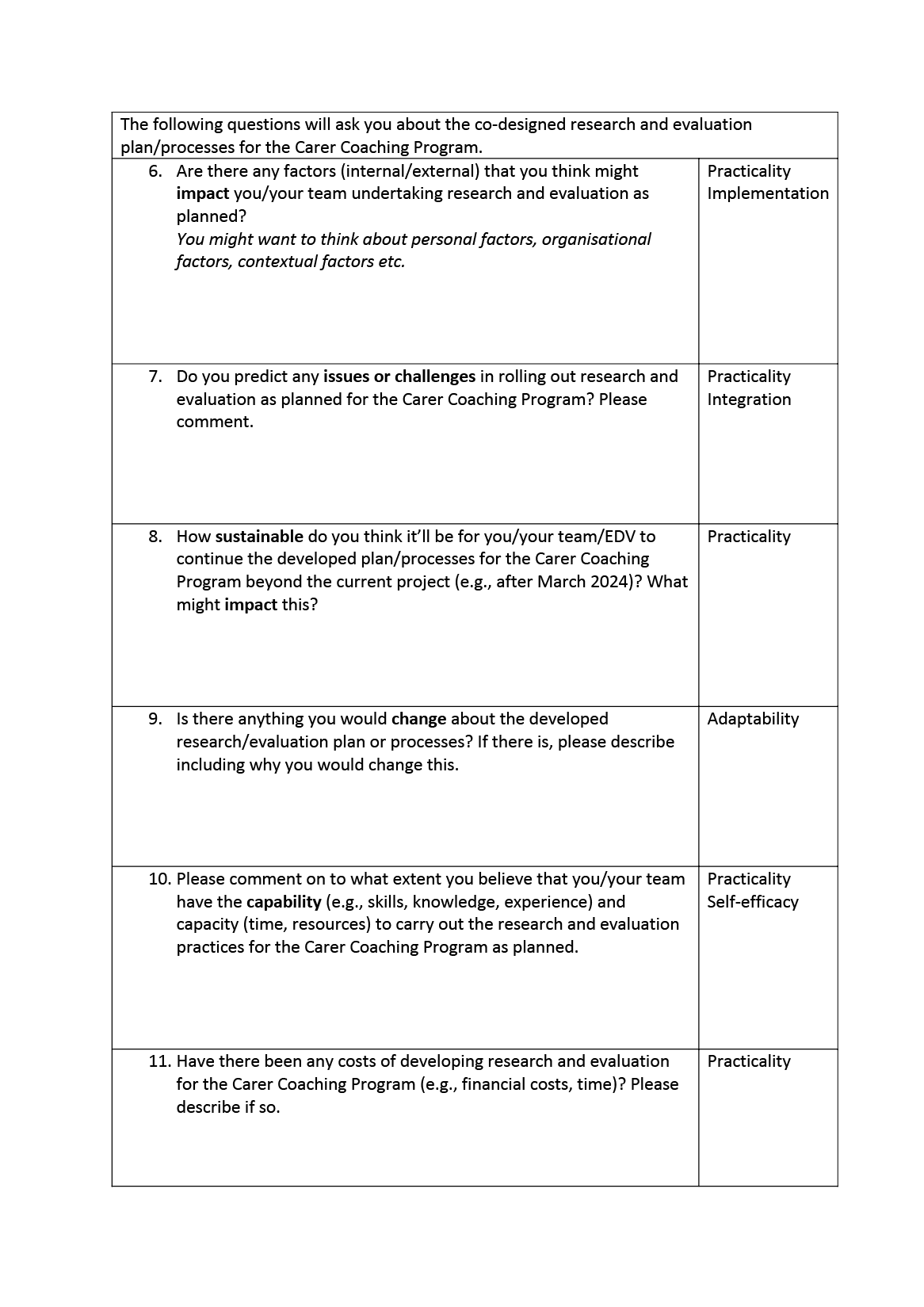
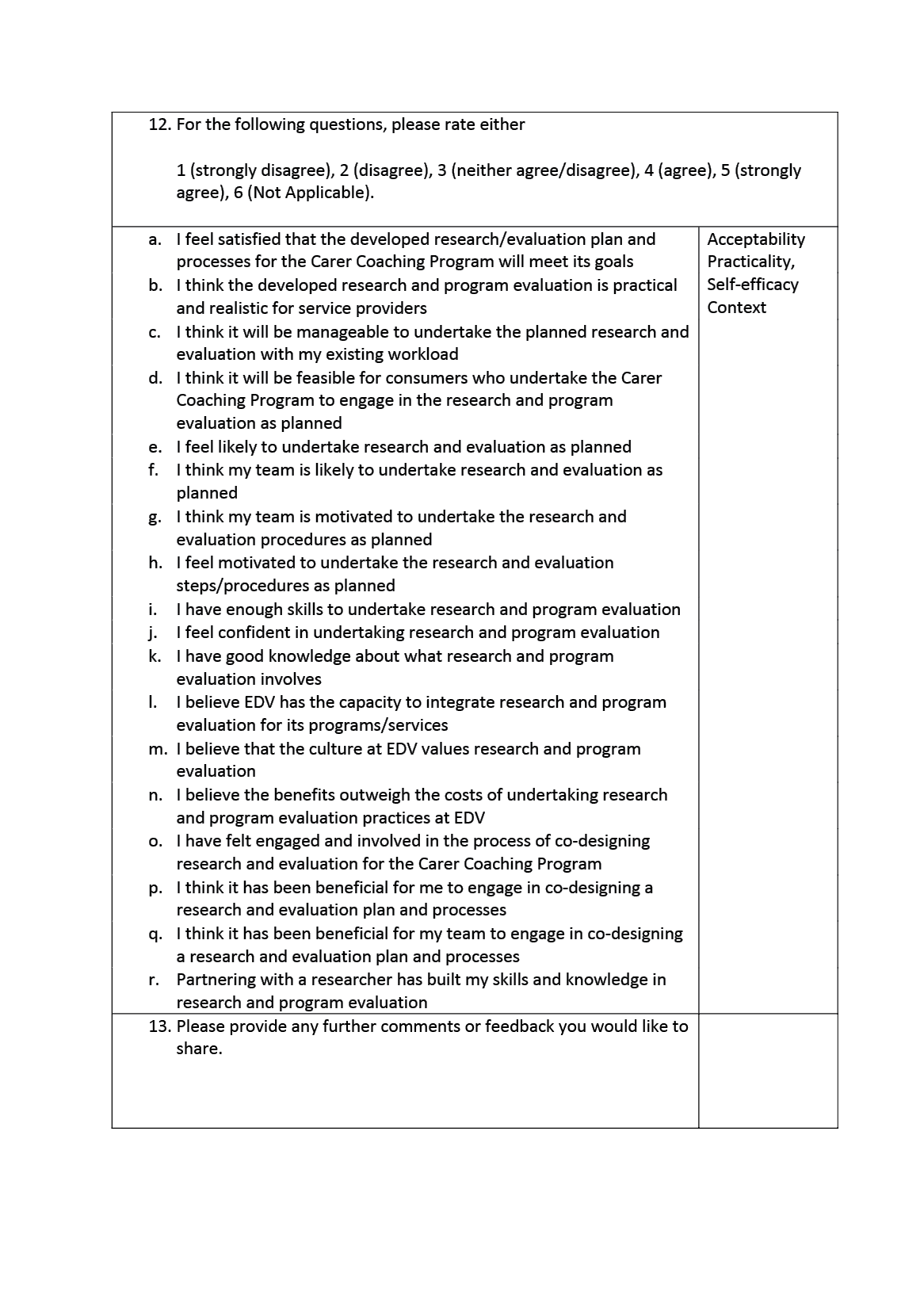
We will follow the NSW Treasury’s (2013) R&E guidelines, making adaptations to available templates (see Appendix 6 for developed templates). This will include developing a program logic, identifying evaluation questions, developing R&E materials and ascertaining staff responsibilities. Prior to implementation, community partners will complete a questionnaire assessing their experiences of co-designing R&E practices (e.g. ‘Overall, how have you found the co-design process of working with others in your team at EDV and a researcher in developing a plan to integrate research and evaluation for the Carer Coaching Program?’ See Appendix 8).
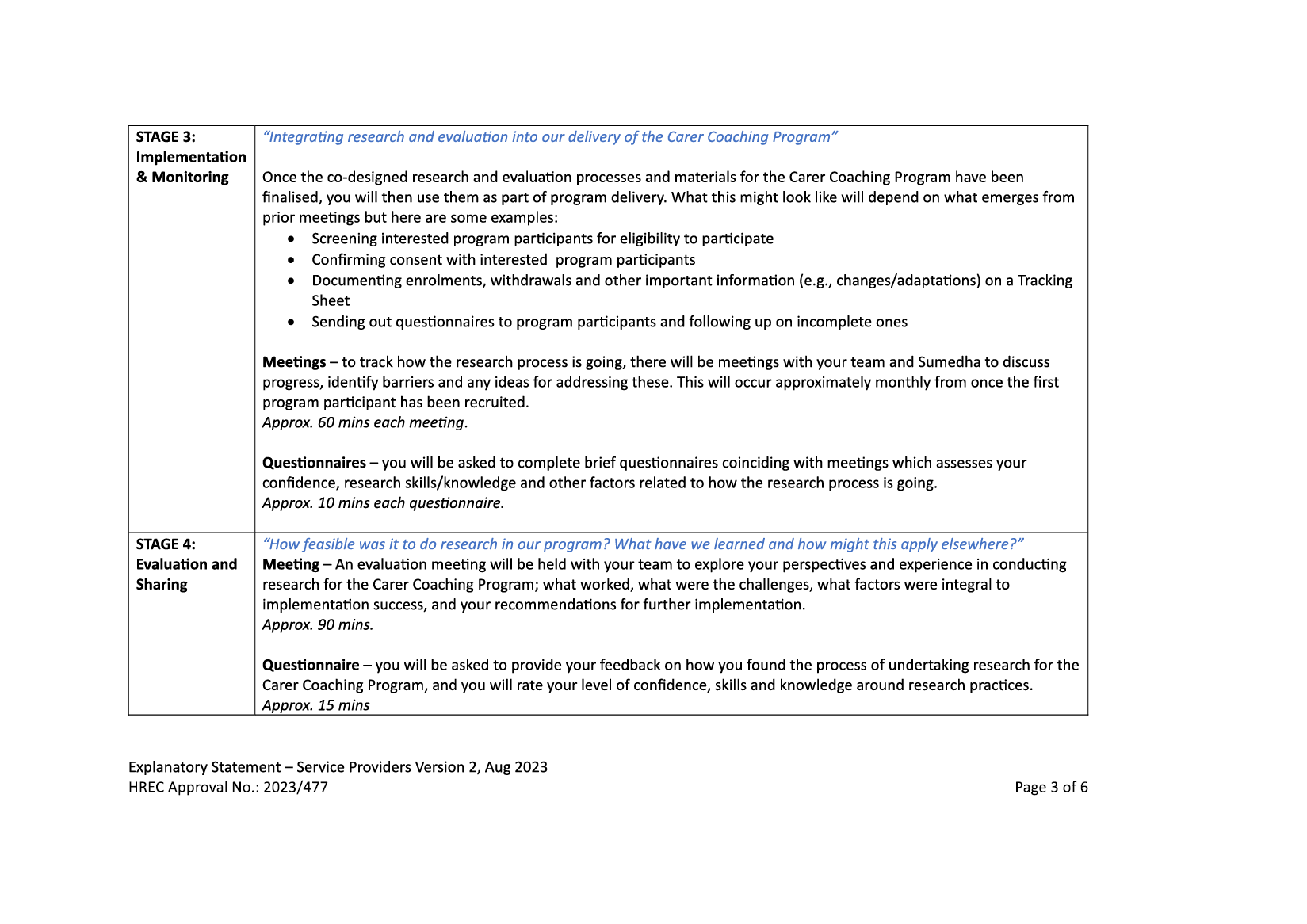
Stage 3: Implementation and Monitoring of Co-designed Research and Evaluation Practices
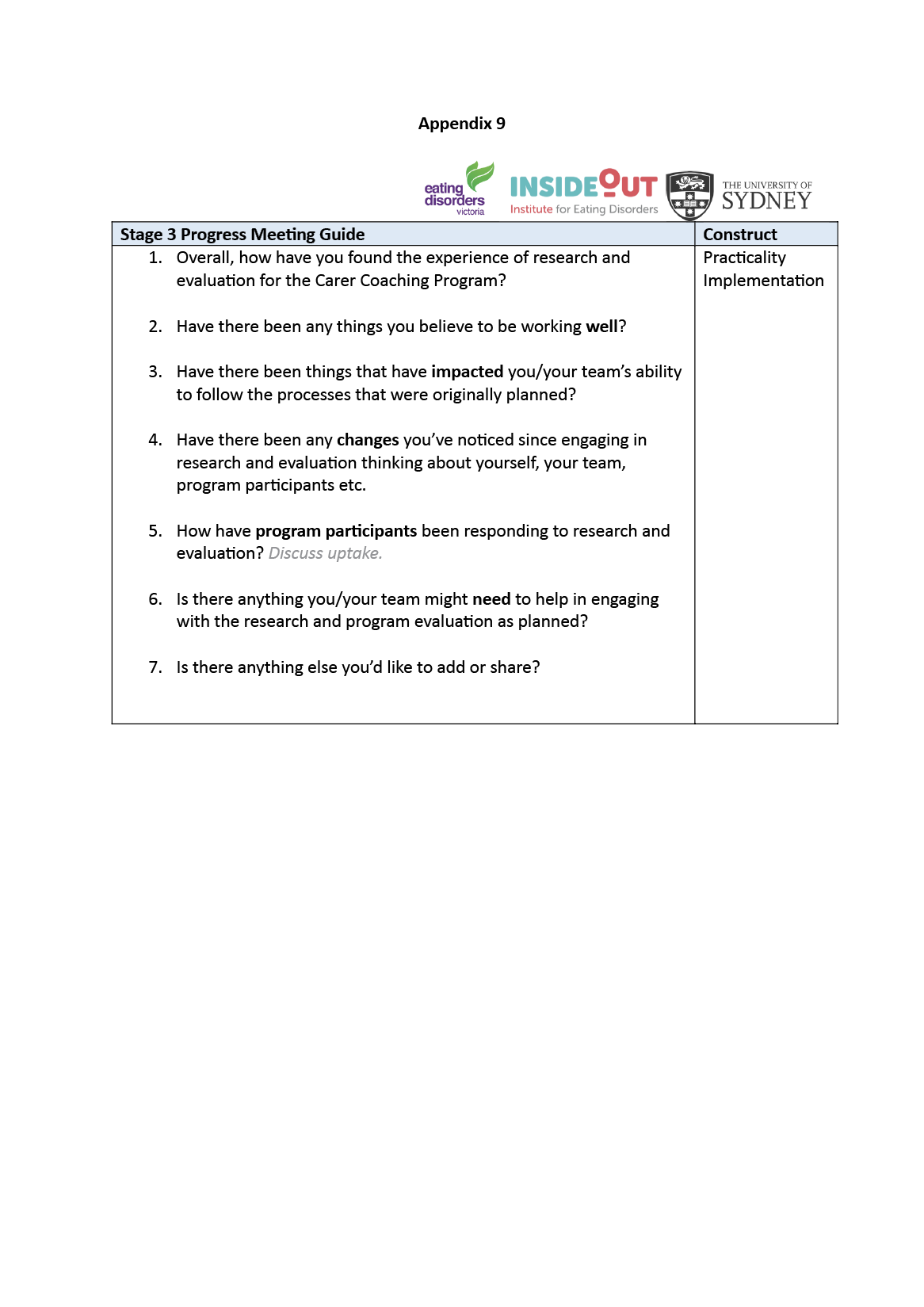
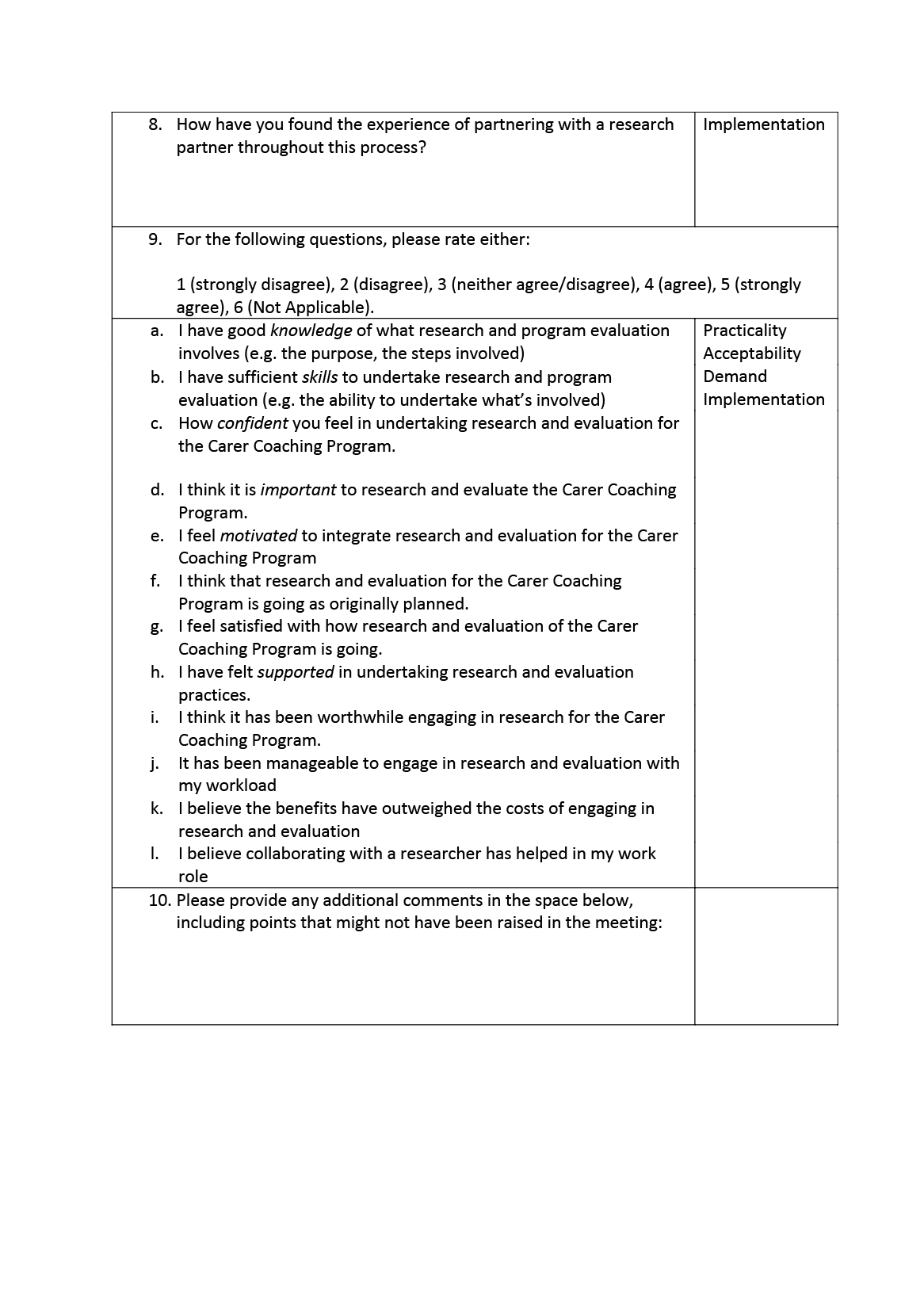
During Stage 3, community partners will implement co-designed R&E practices into service delivery. Monthly meetings will be held, offering opportunities for community and research partners to share experiences and learnings, reflect on the partnership, and discuss impacts, challenges, and any adaptations made to R&E practices (see Appendix 9). Community partners will additionally complete questionnaires assessing implementation and feasibility issues. ‘Have there been any factors that you think may have influenced (positively or negatively) your or your team’s engagement with research and evaluation of the Carer Coaching Program?’; see Appendix 10).
Stage 4: Sharing the Learnings of Co-designing and Engaging in Research and Evaluation
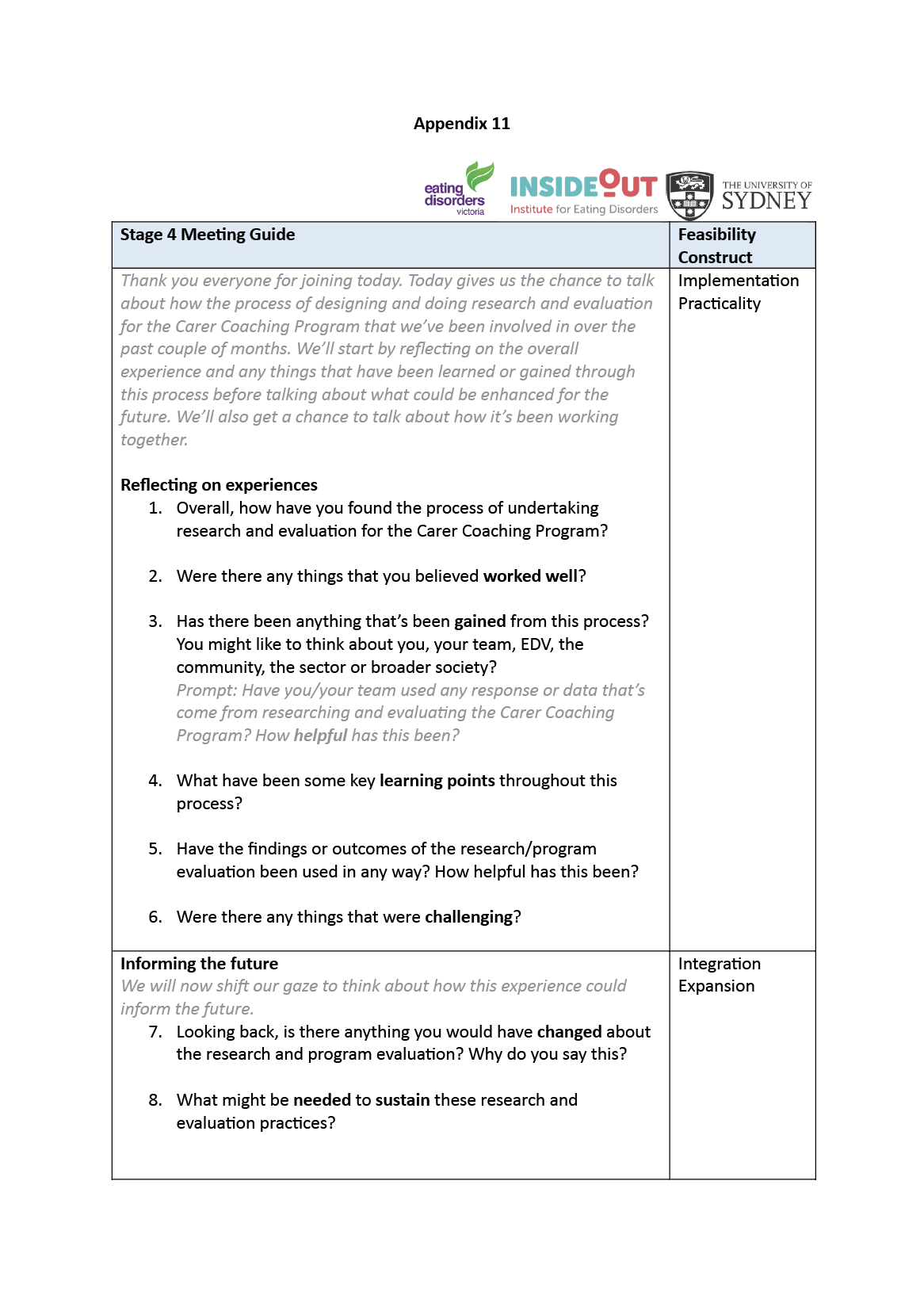
In Stage 4, community and research partners will identify and reflect on the learnings arising from the project. An evaluation meeting will be held with service providers to provide the opportunity to discuss experiences, perceptions and feasibility/sustainability of integrating research and evaluation into service delivery (see Appendix 11). Community partners will also complete an evaluation questionnaire (Appendix 12). We aim to share our experiences and learnings through academic publications, presentations, conferences and newsletters.
Data Analysis
To describe the process and outcomes of the project, selected feasibility and implementation constructs will be assessed, such as acceptability, demand, implementation, practicality and integration (Bowen et al. 2009; Pearson et al. 2020). Data will be analysed using mixed methods, including thematic analysis of meetings/semi-structured interview transcripts, and triangulated with open-ended questionnaire responses and with quantitative data. Meetings/semi-structured interviews will be audio-recorded through the University of Sydney’s Zoom and will be later deidentified. Transcripts will be auto-generated through Zoom artificial intelligence software and manually verified for accuracy by co-authors.
Thematic analysis is a qualitative method for identifying, analysing, organising, describing and reporting themes found within a dataset (Braun & Clarke 2006). It offers a highly flexible approach, providing a rich, yet complex, account of data. This method is intended to yield themes that will provide a more detailed analysis through a combination of inductive and deductive approaches to coding those themes. Analysis will be guided by the six-step thematic analysis framework outlined by Braun and Clarke (2006) which are: (1) familiarising with the data, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes and (6) producing the report. While theme saturation may be used by examining repeating emergent themes (see Fusch & Ness 2015), we recognise the limitations of this method, particularly when undertaking reflexive thematic analysis (Braun & Clarke 2021).
Adverse Events
Community partners will be asked to communicate any adverse events they may experience to the primary research partner. Participants of the Carer Coaching Program will be asked to communicate any adverse events to the Carer Coaches, where they will be managed according to existing organisational protocols. Any adverse events will be reported to the University of Sydney Human Research Ethics Committee.
Data Storage and Management
All data will be password protected and securely stored by co-author Verma and relevant co-investigators on the University of Sydney’s OneDrive for five years and will thereafter be destroyed. A spreadsheet containing participants’ personal details will be stored separately from questionnaire responses. Questionnaires will be linked across time using a personalised alphanumeric code assigned by the primary research partner. Interim data will only be accessible by researchers involved in data collection and analysis. The University of Sydney has a licence to use Qualtrics, a secure online platform, which will provide a basis for release of the explanatory statement, consent form and questionnaires to community partners.
Discussion
This article describes community-based participatory protocol to collaboratively plan for and attempt to build and pilot R&E practices within an Australian community-based eating disorder service through a partnership between service providers and academic researchers. This pragmatic approach jointly aims to address the need for greater R&E within the eating disorder sector, particularly at the community level, while simultaneously identifying features which may assist with facilitating a widespread ecosystem of sustainable, reflexive and equitable R&E practices across the sector into the future.
Community services are a vital source of local knowledge and innovation, yet under-resourcing of R&E activities hinders much needed cross-sectoral translation, policy change and advancement in care. Uplifting R&E at the community level holds several important implications for communities, organisations and systems. First, creating feedback opportunities will help to give voice to those who engage with services to shape organisational policies and procedures, and improve service delivery. Second, establishing routine data collection practices will help us to identify and better understand more diverse eating disorder experiences and recovery trajectories in the community. Third, this process may help inform engagement strategies with marginalised and under-supported groups, particularly First Nations peoples and those from diverse cultural, sexual and gender non-conforming backgrounds, as well as those who identify as men (National Eating Disorders Collaboration 2023; State of Victoria 2023). Fourth, evaluating the effectiveness and efficiency of programs/services will inform funding, scalability and the translation of offerings across services and beyond them to better support community member needs.
Importantly, due to limited resources, our project was restricted by minimal involvement of external lived experience advisers who were unaffiliated with EDV, as well as a relatively short (12-month) project period. While recent research has outlined adaptations for shorter-term community-academic partnerships (Radonic et al. 2023), future projects should prioritise engagement of diverse lived experience perspectives to promote greater equity, community ownership and responsivity.
To the best of our knowledge, this is the first article to outline a plan to connect service providers and academic researchers in an attempt to build R&E within a community eating disorder setting. Through community-engaged methodology, we aim to uplift community service providers to be able to systematically capture, leverage and share data created on the ground through a bottom-up, community-centric approach, while offering research-specific guidance and capabilities. By longitudinally studying the real-time processes and outcomes of partnering to establish and embed R&E praxis within service delivery, we hope that rising insights and learnings will help guide and shape future efforts to feasibly build equitable, reflexive and responsive R&E practices and systems. This will ultimately have implications for enhancing policy, advocacy, prevention and care frameworks to better support people affected by eating disorders and improve the systems around them.
Concluding Thoughts
The preparation and publication of protocols involving pragmatic research methodology like ours presents several benefits. By nature, protocols outline intended processes to achieve certain outcomes based on theoretical underpinnings and decisions made by authoring teams. The early stages of a project’s lifespan offer important knowledge and insights, such as how decisions are made and by whom, and the surrounding contexts which influence how projects are designed, undertaken and arising knowledges ultimately shared.
In writing protocols, authors may gain more clarity around project intentions, processes, gaps and limitations to ultimately strengthen research rigour. They may regularly revisit and reflect on their original plan during and following projects to scaffold insights around what worked, what didn’t, what was learned and what could be changed. This can inform recommendations and advance future research efforts. In tandem, readers may benefit by having access to diverse ways of thinking, resources and structured methodological guidance to spur and enhance their own thinking, processes and recommendations. This specifically addresses the need for greater methodological guidance in undertaking co-design processes in the context of academic partnerships (Benz et al. 2024). Additionally, this could be particularly helpful for early career researchers who may often find themselves within community-based, not-for-profit contexts with limited supports.
Finally, avenues to share pragmatic protocols of community-based research such through open access journals are essential to allow translation of these important knowledges and improve how research is undertaken in the future. This is central to building an ecosystem of accountable, transparent and equitable research praxis, and is only possible by those within the academic community who value, prioritise and continually advocate for greater access and equity.
Acknowledgements
The authors like to acknowledge the Aboriginal and Torres Strait Islander peoples as the traditional custodians of the land upon which this work is being undertaken and wish to pay their respects to Elders past and present. Sovereignty was never ceded. The authors wish to extend their thanks to: Dr Lauren Bruce, Dr Charlotte Young, Dr Gai Moore, A/Prof Yvette Miller, Ms Jess Tone, Dr Sabina Vatter, Dr Shu Hwa Ong, Dr Frank Muscara, Dr Melinda McPherson, Ms Rachel Knight, Prof Steven Allender and Prof Helen Skouteris for their ideas and suggestions in shaping the current project. There is no off-label or investigational use in this study.
References
Ágh, T., Kovács, G., Supina, D., Pawaskar, M., Herman, B. K., Vokó, Z. & Sheehan, D. V. 2016. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eating and Weight Disorders 21, 353-364. https://doi.org/10.1007/s40519-016-0264-x
All-Party Parliamentary Group 2021. Breaking the Cycle: An inquiry into eating disorder research funding in the UK.
April, K., Stenersen, M. R., Deslandes, M., Ford, T. C., Gaylord, P., Patterson, J., Wilson, B. & Kaufman, J. S. 2023. “Give up your mic”: Building capacity and sustainability within community-based participatory research initiatives. American Journal of Community Psychology, 72 203-216. https://doi.org/10.1002/ajcp.12674
Banks, S., Armstrong, A., Carter, K., Graham, H., Hayward, P., Henry, A., Holland, T., Holmes, C., Lee, A., Mcnulty, A., Moore, N., Nayling, N., Stokoe, A. & Strachan, A. 2013. Everyday ethics in community-based participatory research. Contemporary Social Science, 8 263-277. https://doi.org/10.1080/21582041.2013.769618
Benz, C., Scott-Jeffs, W., Mckercher, K. A., Welsh, M., Norman, R., Hendrie, D., Locantro, M. & Robinson, S. 2024. Community-based participatory-research through co-design: supporting collaboration from all sides of disability. Research Involvement and Engagement, 10, 47. https://doi.org/10.1186/s40900-024-00573-3
Berger, P. L. & Luckmann, T. 1967. The Social Construction of Reality: A Treatise in the Sociology of Knowledge, New York, Open Road Integrated Media Inc.
Berkman, N. D., Lohr, K. N. & Bulik, C. M. 2007. Outcomes of eating disorders: a systematic review of the literature. International Journal of Eating Disorders, 40 293-309. https://doi.org/10.1002/eat.20369
Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., Bakken, S., Kaplan, C. P., Squiers, L., Fabrizio, C. & Fernandez, M. 2009. How we design feasibility studies. American Journal of Preventive Medicine, 36, 452-7. https://doi.org/10.1016/j.amepre.2009.02.002
Braun, V. & Clarke, V. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77-101. https://doi.org/10.1191/1478088706qp063oa
Braun, V. & Clarke, V. 2021. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Research in Sport, Exercise and Health, 13 201-216. https://doi.org/10.1080/2159676X.2019.1704846
Bryant, E., Koemel, N., Martenstyn, J. A., Marks, P., Hickie, I. & Maguire, S. 2023. Mortality and mental health funding-do the dollars add up? Eating disorder research funding in Australia from 2009 to 2021: a portfolio analysis. The Lancet Regional Health – Western Pacific, 37. https://doi.org/10.1016/j.lanwpc.2023.100786
Butterfly Foundation 2024. Paying the Price.
Centers for Disease Control and Prevention 1999. Framework for Program Evaluation in Public Health.
Clark, M. T. R., Manuel, J., Lacey, C., Pitama, S., Cunningham, R. & Jordan, J. 2023. Reimagining eating disorder spaces: a qualitative study exploring Māori experiences of accessing treatment for eating disorders in Aotearoa New Zealand. Journal of Eating Disorders, 11 22-22. https://doi.org/10.1186/s40337-023-00748-5
Commonwealth of Australia 2013. A national framework for recovery-oriented mental health services: guide for practitioners and providers.
Conti, J., Joyce, C., Natoli, S., Skeoch, K. & Hay, P. 2021. “I’m still here, but no one hears you”: a qualitative study of young women’s experiences of persistent distress post family-based treatment for adolescent anorexia nervosa. Journal of Eating Disorders, 9, 151. https://doi.org/10.1186/s40337-021-00496-4
Corrigan, P. W. & Oppenheim, M. 2023. The power of community-based participatory research (CBPR). Psychiatric Rehabilitation Journal. https://doi.org/10.1037/prj0000568
Eating Disorders Victoria 2023. Lived Experience and Peer Work Position Paper. Abbotsford, Victoria.
Farmer, E. A. & Weston, K. M. 2002. A conceptual model for capacity building in Australian primary health care research. Australian Family Physician, 31 12, 1139-42.
Fletcher, L., Trip, H., Lawson, R., Wilson, N. & Jordan, J. 2021. Life is different now - impacts of eating disorders on Carers in New Zealand: a qualitative study. Journal of Eating Disorders, 9, 91. https://doi.org/10.1186/s40337-021-00447-z
Fusch, P. & Ness, L. 2015. Are We There Yet? Data Saturation in Qualitative Research. Qualitative Report 20, 1408. https://doi.org/10.46743/2160-3715/2015.2281
Gisladottir, M., Treasure, J. & Svavarsdottir, E. K. 2017. Effectiveness of therapeutic conversation intervention among caregivers of people with eating disorders: quasi‐experimental design. Journal of Clinical Nursing 26, 735-750. https://doi.org/10.1111/jocn.13412
Golenko, X., Pager, S. & Holden, L. 2012. A thematic analysis of the role of the organisation in building allied health research capacity: a senior managers’ perspective. BMC Health Services Research, 12 276. https://doi.org/10.1186/1472-6963-12-276
Grennan, L., Nicula, M., Pellegrini, D., Giuliani, K., Crews, E., Webb, C., Gouveia, M.-R., Loewen, T. & Couturier, J. 2022. “I’m not alone”: a qualitative report of experiences among parents of children with eating disorders attending virtual parent-led peer support groups. Journal of Eating Disorders, 10, 195-195. https://doi.org/10.1186/s40337-022-00719-2
Guijt, I. M. 2014. Participatory Approaches. Methodological Briefs: Impact Evaluation 5. Florence, Italy: UNICEF Office of Research.
Hamilton, A., Mitchison, D., Basten, C., Byrne, S., Goldstein, M., Hay, P., Heruc, G., Thornton, C. & Touyz, S. 2022. Understanding treatment delay: Perceived barriers preventing treatment-seeking for eating disorders. Australian and New Zealand Journal of Psychiatry, 56 248-259. https://doi.org/10.1177/00048674211020102
Hay, P., Aouad, P., Le, A., Marks, P., Maloney, D., Touyz, S. & Maguire, S. 2023. Epidemiology of eating disorders: population, prevalence, disease burden and quality of life informing public policy in Australia-a rapid review. Journal of Eating Disorders, 11 23. https://doi.org/10.1186/s40337-023-00738-7
Insideout Institute 2021. Australian Eating Disorders Research & Translation Strategy 2021-2031. Sydney, Australia: University of Sydney.
Israel, B. A., Eng, E., Parker, E. A. & Schulz, A. J. 2012. Methods for Community-Based Participatory Research for Health, Newark, Newark: Jossey-Bass.
Israel, B. A., Schulz, A. J., Parker, E. A., Becker, A. B., Allen, A. J., Iii, Guzman, J. R. & Lichtenstein, R. 2018. Critical Issues in Developing and Following CBPR Principles. In: DURAN, B., WALLERSTEIN, N., OETZEL, J. G. & MINKLER, M. (eds.) Community-Based Participatory Research for Health: Advancing Social and Health Equity Third edition ed. Hoboken, NJ: Jossey-Bass and Pfeiffer Imprints, Wiley.
Janesick, V. J. 1999. A Journal About Journal Writing as a Qualitative Research Technique: History, Issues, and Reflections. Qualitative Inquiry, 5, 505-524. https://doi.org/10.1177/107780049900500404
Johns, G., Taylor, B., John, A. & Tan, J. 2019. Current eating disorder healthcare services - the perspectives and experiences of individuals with eating disorders, their families and health professionals: systematic review and thematic synthesis. BJPsych Open, 5, e59. https://doi.org/10.1192/bjo.2019.48
Jull, J., Giles, A. & Graham, I. D. 2017. Community-based participatory research and integrated knowledge translation: advancing the co-creation of knowledge. Implementation Science, 12, 150. https://doi.org/10.1186/s13012-017-0696-3
Karlstad, J., Moe, C. F., Adelsten Stokland, R. & Brinchmann, B. S. 2022. “Balancing within a closed family system”: a grounded theory study of how family life is affected by having a family member with an eating disorder. Journal of Eating Disorders, 10, 147. https://doi.org/10.1186/s40337-022-00669-9
Kaufman, J. S., Abraczinskas, M. & Salusky, I. S. 2020. Tell it to Me Straight: The Benefits (and Struggles) of a Consumer-driven Assessment Process. American Journal of Community Psychology, 65, 125-135. https://doi.org/10.1002/ajcp.12373
Kurnik Mesarič, K., Damjanac, Ž., Debeljak, T. & Kodrič, J. 2024. Effectiveness of psychoeducation for children, adolescents and caregivers in the treatment of eating disorders: A systematic review. European Eating Disorders Review, 32, 99-115. https://doi.org/10.1002/erv.3028
Lewis, H. K. & Foye, U. 2021. From prevention to peer support: a systematic review exploring the involvement of lived-experience in eating disorder interventions. Mental Health Review Journal 27, 1-17. https://doi.org/10.1108/MHRJ-04-2021-0033
Lincoln, Y. S. & Guba, E. G. 1985. Naturalistic inquiry, Beverly Hills, California, Sage Publications. https://doi.org/10.1016/0147-1767(85)90062-8
Mcardle, S. 2019. Parents’ experiences of health services for the treatment of eating disorders: a qualitative study. Journal of Mental Health 28, 404-409. https://doi.org/10.1080/09638237.2017.1417558
Merriam, S. B. & Brockett, R. G. 2007. The profession and practice of adult education : an introduction, San Francisco; United States, Jossey-Bass Publishers.
Minkler, M. & Wallerstein, N. 2008. Community-based participatory research for health from process to outcomes, San Francisco, CA, Jossey-Bass.
Miskovic-Wheatley, J., Bryant, E., Ong, S. H., Vatter, S., Le, A., Aouad, P., Barakat, S., Boakes, R., Brennan, L., Bryant, E., Byrne, S., Caldwell, B., Calvert, S., Carroll, B., Castle, D., Caterson, I., Chelius, B., Chiem, L., Clarke, S., Conti, J., Crouch, L., Dammery, G., Dzajkovski, N., Fardouly, J., Felicia, C., Feneley, J., Firriolo, A.-M., Foroughi, N., Fuller-Tyszkiewicz, M., Fursland, A., Gonzalez-Arce, V., Gouldthorp, B., Griffin, K., Griffiths, S., Hambleton, A., Hannigan, A., Hart, M., Hart, S., Hay, P., Hickie, I., Kay-Lambkin, F., King, R., Kohn, M., Koreshe, E., Krug, I., Linardon, J., Long, R., Long, A., Madden, S., Maguire, S., Maloney, D., Marks, P., Mclean, S., Meddick, T., Miskovic-Wheatley, J., Mitchison, D., O’kearney, R., Ong, S. H., Paterson, R., Paxton, S., Pehlivan, M., Pepin, G., Phillipou, A., Piccone, J., Pinkus, R., Raykos, B., Rhodes, P., Rieger, E., Rodan, S.-C., Rockett, K., Russell, J., Russell, H., Salter, F., Sawyer, S., Shelton, B., Singh, U., Smith, S., Smith, E., Spielman, K., Squire, S., Thomson, J., Touyz, S., Utpala, R., Vartanian, L., Vatter, S., Wallis, A., Ward, W., Wells, S., Wertheim, E., Wilksch, S., Williams, M., Touyz, S., Maguire, S. & National Eating Disorder Research, C. 2023. Eating disorder outcomes: findings from a rapid review of over a decade of research. Journal of Eating Disorders, 11, 85. https://doi.org/10.1186/s40337-023-00801-3
Morton, M., Bergen, A., Crann, S., Bader, D., Horan, M. & Bonham, L. 2014. Engaging evaluation research: Reflecting on the process of sexual assault/domestic violence protocol evaluation research. Gateways: International Journal of Community Research and Engagement, 7, 1-17. https://doi.org/10.5130/ijcre.v7i1.3395
National Eating Disorders Collaboration 2019. Peer Work Guide.
National Eating Disorders Collaboration 2023. National Eating Disorders Strategy 2023-2033.
New South Wales Treasury 2013. Policy and Guidelines: Evaluation.
Overton, M. D. 2017. Conceptualizing a Theoretical Framework: Embodied Narrative Knowing. Proceedings of the 3rd International Conference on Higher Education Advances. https://doi.org/10.4995/HEAD17.2017.5557
Pearson, N., Naylor, P. J., Ashe, M. C., Fernandez, M., Yoong, S. L. & Wolfenden, L. 2020. Guidance for conducting feasibility and pilot studies for implementation trials. Pilot and Feasibility Studies, 6, 167. https://doi.org/10.1186/s40814-020-00634-w
Peralta, K. & Murphy, J. 2016. Community-Based Participatory Research and the Co-Construction of Community Knowledge. The Qualitative Report 21, 1713-1726. https://doi.org/10.46743/2160-3715/2016.2526
Radonic, L., Jacob, C., Kalman, R. & Lewis, E. Y. 2023. It’s a sprint, not a marathon: a case for building short-term partnerships for community-based participatory research. Qualitative Research 23, 380-398. https://doi.org/10.1177/14687941211029477
Reed, R. 2015. Program evaluation as community-engaged research: Challenges and solutions. Gateways: International Journal of Community Research and Engagement, 8, 118-138. https://doi.org/10.5130/ijcre.v8i1.4105
Regan, P., Cachelin, F. M. & Minnick, A. M. 2017. Initial treatment seeking from professional health care providers for eating disorders: A review and synthesis of potential barriers to and facilitators of “first contact”. International Journal of Eating Disorders, 50, 190-209. https://doi.org/10.1002/eat.22683
Robinson, T., Bailey, C., Morris, H., Burns, P., Melder, A., Croft, C., Spyridonidis, D., Bismantara, H., Skouteris, H. & Teede, H. 2020. Bridging the research–practice gap in healthcare: a rapid review of research translation centres in England and Australia. Health Research Policy and Systems, 18, 117. https://doi.org/10.1186/s12961-020-00621-w
Sadler, L. S., Larson, J., Bouregy, S., Lapaglia, D., Bridger, L., Mccaslin, C. & Rockwell, S. 2012. Community–University Partnerships in Community-Based Research. Progress in Community Health Partnerships, 6, 463-469. https://doi.org/10.1353/cpr.2012.0053
Solhaug Storli, C. & Alsaker, S. 2021. Treatment of eating disorders: voices from a ward. International Journal of Qualitative Studies on Health and Well-being, 16, 1983948. https://doi.org/10.1080/17482631.2021.1983948
State of Victoria 2023. Victorian eating disorders strategy: What we heard report. Melbourne, Victoria.
Truttmann, S., Philipp, J., Zeiler, M., Franta, C., Wittek, T., Merl, E., Schöfbeck, G., Koubek, D., Laczkovics, C., Imgart, H., Zanko, A., Auer-Welsbach, E., Treasure, J., Karwautz, A. F. K. & Wagner, G. 2020. Long-Term Efficacy of the Workshop Vs. Online SUCCEAT (Supporting Carers of Children and Adolescents with Eating Disorders) Intervention for Parents: A Quasi-Randomised Feasibility Trial. Journal of Clinical Medicine, 9. https://doi.org/10.3390/jcm9061912
Utpala, R., Squire, S. & Farrar-Rabbidge, M. 2023. Eating Disorders Peer Workforce Guidelines. Sydney, Australia: Butterfly Foundation.
Wallerstein, N. B. & Duran, B. 2006. Using community-based participatory research to address health disparities. Health Promotion Practice, 7, 312-23. https://doi.org/10.1177/1524839906289376
Wilson, E. 2019. Community-Based Participatory Action Research. In: LIAMPUTTONG, P. (ed.) Handbook of Research Methods in Health Social Sciences. Singapore: Springer Singapore. https://doi.org/10.1007/978-981-10-5251-4_87